By Eirik Garnas
www.OrganicFitness.com
“All disease begins in the gut”
– Hippocrates
About 2000 years after the father of medicine said these words, the emerging field of microbiome science and increased focus on the gastrointestinal tract in health and disease have revealed that Hippocrates was probably right all along. Of course, saying that all disease begins in the gut is clearly stretching the truth, but science shows that it’s definitely ground zero for a lot of the ills that run rampant in the modern world. Since around 70% of our immune system is located in and around the gastrointestinal tract, it’s clear that taking good care of the digestive machinery is a good idea if you want to live a long and healthy life. Also, besides the obvious impact on general health, good gut health is also of special interest to those who are interested in fitness, as it in many ways is a key to optimizing workout results.

Good gut health isn’t only a key to a long and healthy life, it also lays the foundation for optimal athletic performance. Picture: Christina Gloger
While the discussion surrounding nutrition and exercise long has revolved around adequate protein intake, post-workout food intake, carbohydrates vs. fats, etc., we’re now starting to understand that macronutrient composition and nutrient timing are only a part of the picture. Since the food you eat is what fuels your efforts in the gym, and a healthy gut microbiota (the collection of microbes that live in the GI tract) promotes a well functioning immune system, making sure gut health is taken care of is especially important for athletes and fitness enthusiasts who want to boost recovery and athletic performance. Studies in animals even show that beneficial bacteria can significantly increase testosterone production (1), and although we need human data to confirm that these results also apply to our species, there’s no doubt that the increased production of short-chain fatty acid’s in the colon, decreased low-grade inflammation, and improved metabolic health that result from boosting gut health have a positive impact on physical fitness.
Just like trainees should eat a diet that optimizes gene expression in the human genome, paying attention to the vastly larger (in terms of unique genetic material) human microbiome (the collective genomes of all the microbes that live in and on the human body) is also essential. However, as it turns out, a lot of the things we have to do to optimize human gene expression, are also the things we have to do to take good care of the second genome in our body.
If we’re really going to optimize athletic performance and muscle growth, we have to focus not just on our human cells and DNA, but also on our microbial inhabitants and the DNA they provide.
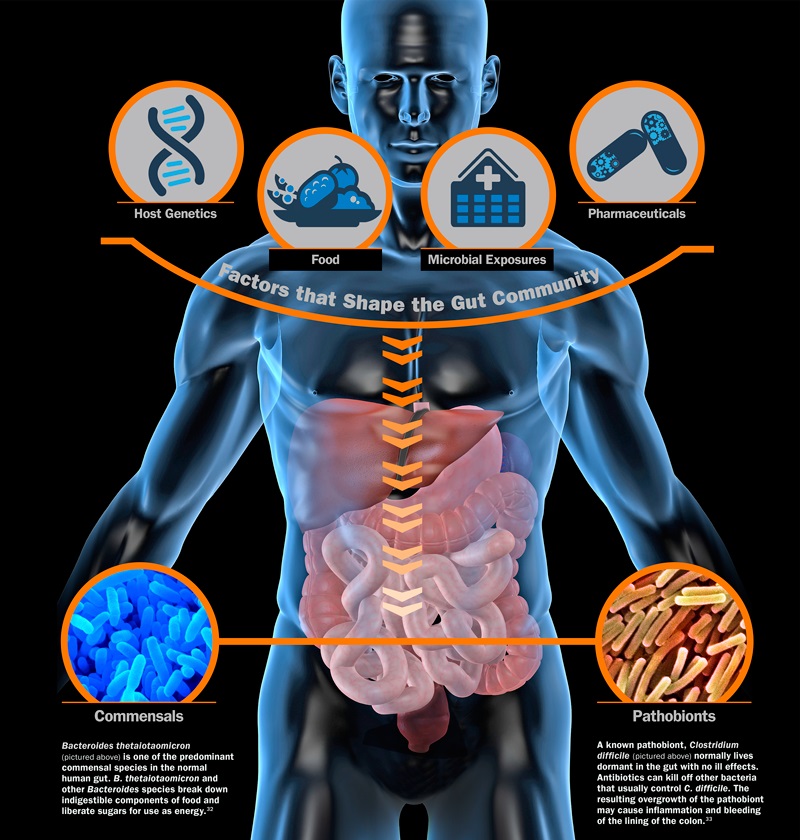
The complex ecosystem in our gut and the vital role of the intestinal barrier
The human body is inhabited by trillions of microorganisms from thousands of different species, but it’s only during the last 5-10 years that we’ve really begun to understand the essential role these critters play in our health. To get a scope of the magnitude of this microbial rainforest, it’s now clear that the vast majority of cells in our body are microbial and that these germs provide us with 99% of our total genetic material (2,3). This alone is enough to understand that we can no longer dismiss human-microbe contact as simply a question of pathogens and infectious disease, but that we have to start looking at Homo sapiens as a superorganism that is made up of both eukaryotic and prokaryotic cells.
Most of these critters live in our gastrointestinal tract, where they help us digest food, regulate our immune system, and provide a wide spectrum of other functions that researchers are just beginning to explore. This gut microbiota is often referred to as the forgotten organ; an essential piece of the human body that has long been dismissed, but is now starting to gain massive attention in both the scientific community and popular press.
One of the most important functions of these gut microbes is to help control the absorption of luminal content through the gut wall. The intestinal barrier is the main interface between us and the external environment, and this barrier is essentially outside our body, in the sense that the gut is constantly bombarded with antigens, bacteria, food, and other components from the environment.
While there’s still a way to go in terms of establishing cause and effects in a lot of health problems, a plethora of chronic health disorder have now been scientifically linked to a dybiotic gut microbiota (microbial imbalances), loss of microbial old friends, and/or leaky gut (increased intestinal permeability). While both gut dysbiosis and leaky gut were once considered bogus/alternative disorders, there are now thousands of scientific papers linking these conditions to diseases such as type-2 diabetes (4), cardiovascular disease (5), acne vulgaris, and obesity (6).
Saving the human microbiome
Ironically enough, the primary reason we now have to use science to learn more about how to manipulate the microbiome is that modern technology and science have allowed us to create foods, drugs, and living conditions that perturb the microbial ecosystems that live in and on our bodies. In a healthy state, we provide gut bacteria with food and shelter, they provide us with functions that stretch far beyond the scope of our own physiological capabilities, and our human and microbial part live silently and symbiotically side by side. However, the so-called westernized microbiome, damaged by antibiotics, caesarean sections, refined foods, and sterile living conditions, doesn’t shield us from disease in the same way as the hunter-gatherer microbiome (7,8,9).
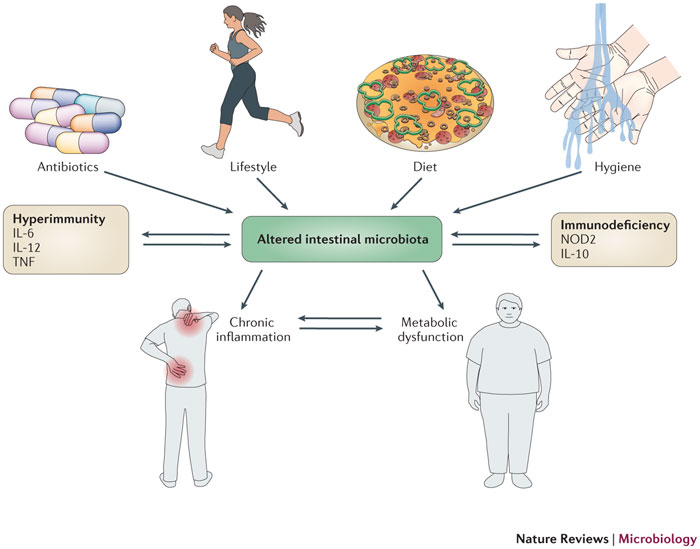
The western lifestyle perturbs the human microbiome .Image source
To restore a natural equilibrium we have to return to our roots and understand that just like our human genome was forged in an ancestral natural environment, the microbiome is also healthiest when we eat nutritious whole foods, drink clean (non-chlorinated) water, spend time outdoors, perform natural births, breastfeed infants, get dirty once in a while, and take other measures to populate the microbiota with new types of bacteria and feed healthy microbial populations. While several lifestyle factors impact the microbiome, the following 4 are especially important for boosting good bacterial populations and tightening up the intestinal junctions that have become “loose”.
1) Eat traditionally fermented foods
It’s important to note that I’m not talking about the low-fat acidophilus milk you’ll find at the average grocery store. Instead we’re aiming for products such as dirty fermented veggies, grass-fed greek yoghurt, and thousand of years old kefir grains. Traditionally fermented foods are a rich bacterial resource and also provide other food ingredients – such as vitamin K in sauerkraut and lactoferrin in kefir – which are often lacking from the modern diet (10). Make your own or take a trip down to your closest health food store (make sure you get raw and fermented) and pick up some of nature’s “superfood”.
2) Eat more fermentable substrates/prebiotics
While fermented foods and other sources of probiotics help populate the gut microbiota with good bugs like lactobacillus and bifidobacteria, these guys won’t set up shop in your GI tract unless they are given the proper fuels to survive and thrive. The human genome only produces the necessary enzymes to break down some proteins, fats, simple sugars, and starch, but the gut microbiome can adapt to break down a wide range of food ingredients. Certain indigestible (to the human host) compounds, such as inulin-type fructans and resistant starches, are especially beneficial as they specifically boost populations of good bacteria. However, the key here is to already have a relatively healthy gut ecosystem to begin with, as supplementing with heavy doses of prebiotics in an imbalanced (dysbiotic) gut could do more harm than good. Combining prebiotics with sources of probiotics such as traditionally fermented foods is therefore especially important if you’re suffering from moderate-severe gut dysbiosis.
Good sources of inulin-type fructans include leeks, onions, and jerusalem artichoke. Resistant starch is found in green bananas, legumes, and potatoes, among other foods. As cooking breaks down a lot of the resistant starch found in food, cooling legumes and potatoes for about 36 hours after heating is a good approach. This increases the resistant stach content through a process called starch retrogradation. Potato starch in its raw form has become especially popular lately, as it is a cheap and convenient source of gut friendly resistant starch.
It’s estimated that most contemporary hunter-gatherers and paleolithic tribes have/had vastly more fermentable substrates in their diet compared to what is found in the refined western diet.
Overall message: Eat more plants, and especially those that are rich in fermentable substrates/prebiotics. Fermentable substrates boost the growth of beneficial bacteria and production of short-chain fatty acids in the colon and allow your gastrointestinal barrier to function optimally (11,12,13).
3) Stay clear of antibiotics and other antimicrobial drugs if possible
There’s now overwhelming evidence showing that the rampant use of antimicrobials both in humans, livestock, and farming changes the microbial ecosystems in our environment (14,15,16). While antibiotics certainly have helped the human race overcome several types of infectious diseases, they also wipe out good gut bacteria and can thereby promote a state of gut dysbiosis.
As previously mentioned, researchers are now beginning to talk about a westernized microbiome, which diversity and resilience is nothing more than a faint imprint of the ancestral microbiome of our ancestors – or even just people who lived before the antibiotic era. Modern hygiene, western diets, and a lack of microbial exposures have certainly contributed to this ecosystem disaster, but broad spectrum antibiotics play an especially important role as they are like a carpet bomb to the gut microbiome.
4) Get dirty
Soaps, antibacterial gels, and cleaning detergents are all considered an essential part of the civilized, modern lifestyle. However, let’s forget the TV commercials and magazine ads extolling the virtues of regular hand washing and clean homes and look back at the way humans have lived throughout most of our evolutionary history. Food with clinging soil, untreated water, and a raw and animal-like contact with nature are all part of the evolutionary milieu in which our genome was forged, and although we’ve now disconnected ourselves from these exposures, it doesn’t mean that we have adapted to extremely “clean” living conditions.
While we’ve known for a long time that indoor living and lack of sun exposure lead to “inferior” gene expression in our human genome, we’re now learning that the consequences to our microbiome could be even greater. By “shutting off” contact to the vast microbial ecosystems found in the environment around us, such as in unpolluted and untreated water and soil, we’ve also distanced ourselves from some old microbial friends.
Nobody’s denying that modern hygiene has helped us overcome life-threatening infectious diseases and that life in the industrialized world has many upsides. However, it’s also important to note that this disconnect from mother nature has significant implications for human heath. The hygiene hypothesis, which states that a lack of microbial exposure in early stages of life leads to poor immunoregulation and increased risk of autoimmune disease later in life, has now gotten its successor in the old friends hypothesis. This hypothesis, which is supported by more and more compeling evidence, states that a lack of microbial exposures leads to higher risk of disease because we’re losing contact with “microbial old friends” that once were a part of the diverse, ancestral human microbiome.
Several studies are now beginning to show that contemporary hunter-gatherers and non-westernized populations have vastly more diverse microbiomes than westerners, and it’s likely that this is one of the primary reasons these cultures have such low incidence of inflammatory health disorders (17,18,19).
Summary/takeaway
Diseases of civilization, such as type-2 diabetes, obesity, and cardiovascular disease, are also sometimes called mismatch diseases (20). This means that they primarily result from a gene-environment mismatch, in the sense that our genome hasn’t adapted to the modern lifestyle that is characterized by sedentary living, the western dietary pattern, widespread use of pharmaceuticals, etc. However, we’re now learning that this mismatch doesn’t only involve the human genome, but also the vastly larger human microbiome (the collective genomes of all the microbes that live in and on the human body).
The human microbiome responds rapidly to changes in environment and lifestyle, and it’s now well established that the typical western lifestyle perturbs the microbial ecosystems in and on our body. Most of the critters associated with the human host live in the gastrointestinal tract, and this gut microbiota – the collection of microbes in our GI tract – plays an especially important role in health and disease. As gut bacteria regulate our immune system, impact hormone production, and break down the food we eat, a healthy gut microbiota is also essential for good athletic performance and recovery.
So, how can we deal with this mismatch? Do we have to move into the wilderness and adopt a hunter-gatherer lifestyle? No, unless that’s your thing of course. However, dirtying up our modern lifestyle by reconnecting with nature, adopting ancient food practises, and rewilding our bodies is something everyone can benefit from. From a practical standpoint, eating a healthy diet is the number one key to good gut health. Besides this top priority, eating more traditionally fermented foods and fermentable substrates, avoiding antibiotics, and getting dirty once in a while are 4 of the major things that you can incorporate into your lifestyle today.
About the author
 Name: Eirik Garnas
Name: Eirik Garnas
Website: www.OrganicFitness.com
![]() Besides studying for a degree in Public Nutrition, Iíve spent the last couple of years coaching people on their way to a healthier body and better physique. I’m educated as a personal trainer from the Norwegian School of Sport Sciences and also have additional courses in sales/coaching, kettlebells, body analysis, and functional rehabilitation. Subscribe to my website and follow my facebook page if you want to read more of my articles on fitness, nutrition, and health.
Besides studying for a degree in Public Nutrition, Iíve spent the last couple of years coaching people on their way to a healthier body and better physique. I’m educated as a personal trainer from the Norwegian School of Sport Sciences and also have additional courses in sales/coaching, kettlebells, body analysis, and functional rehabilitation. Subscribe to my website and follow my facebook page if you want to read more of my articles on fitness, nutrition, and health.




Excellent article. Other than the beneficial foods mentioned, is there a wider list of basic, whole foods that we can add to our diet to help keep our gut healthy?
Barry, take a look at some of mye previous articles on nutrition, which cover what to eat! http://organicfitness.com/category/diet/
These are all general recommendations that make sense. It’s important to understand that sugar and grains increase the growth of candida albicans. This creates intestinal dysbiosis, which leads to an unhealthy gut and auto – immune disease. This is part of the reason why people today have such high levels of auto immune and digestive issues.
It’s just amazing Eric, that you can trace everything back to when we became a civilized society. Ever time i read something of yours, i learn something. Thank you.
Happy to hear it Shane!
Erik I’ve had this pain before on my inner left glute that got me thinking that could be Sciatica. Others have told me that you can get similar pain from getting some inner deep muscles on the glute inflamed. How can I tell apart one from the other?
Not sure John. You should probably get Bret’s opinion on that.
I began fermenting and making my own milk kefir a little over a year ago. I definitely noticed my general health has been better over the last year. I usually get a cold every winter anywhere for a few days to a week and I didn’t get one at all this winter (and it was a long one here in the northeast!). Without getting too visual, I’ve also noticed my bowel movements are much more regular as well.
Seriously? Is this article really extolling the virtues of hepatitis A and polio? Because that’s what you get when you ingest contaminated water. I’m pretty sure infant and maternal mortality are much higher in developing countries where they perform very few c-sections and deliver in “natural” conditions in comparison to the US. Sorry, but this article reads like uneducated fear mongering ala Jenny McCarthy, without the acknowledgement of real world epidemiological data. Do you know why my 1 year old son was exposed to mumps in daycare, threatening his fertility? It’s because uneducated parents who espouse the magic of “natural” living refuse to immunize their children, and threaten the protective effect of herd immunity.
I’m not saying that Western society has the optimal diet. But articles like this are irrational and discount 100 of years of positive human innovation and promote fanatical, divisive ideologies.
For the record, I love this blog and have purchased the 2×4 program the first day it came out. The reason I love this blog is Bret’s evidence based and scientifically grounded advice on how to live a stronger and healthier life.
Nobody’s advocating drinking contaminated water. What I wanted to emphasise in the article is that there are now plenty of data showing that the focus on cleanliness (i.e., hand sanitizers, antibacterials, chlorination) in the western world comes with some hidden costs.
How can a immunized child get threatened through an un-immunized child? Does the immunization not work? How can a new born child get hepatitis A when not having sex or blood transfusion? And who is drinking contaminated (whith what by the way) water? Why is the mortality in undeveloped countries so much higher even though they are immunized much more and with higher dosages than western society? And what does real world epidemiological data is about? This data is manipulated and taken out of the wrong relation! This is no secret anymore! People get paid a huge amount of money to lie and to fake data! And what is the positive human innovation all about if we have every year more and more obesity, diabetes, cancer, chronic conditions, pain, drug abuse, dialysis, vaccine victims, auto-immune-disease etc.? I can’t see any progress to a better for humans, not at all!
Hi Eirik!
Love your articles.
Where do you stand on raw apple cider vinegar?
Keep up the good work.
Glad to hear it!
For what purpose?
I was diagnosed with acid reflux and was taking 40 mg of pantoprazole. It was suggested to me, by a family member who is an RN, that ACV would treat the reflux, and I could stop the meds. I tried it (1 Tbsp in a small glass of water) and it worked! I started reading about it, and it is allegedly a “prebiotic”, a food that feeds good bacteria. I was wondering, as you are well educated in nutrition, if you could say how this ranks compared to the suggested foods you’ve recommended (kefir, grass-fed yogurt, etc.)
Congrats on getting rid of the acid reflux! Not aware of any studies investigating the prebiotic properties of ACV. However, it does contain pectin, a carbohydrate that is believed to feed good bacteria in the gut.