Hello blog readers! I have a great week of blogposts planned so make sure you check back later in the week. Today is an interview with Jurdan Mendigutxia. Tomorrow will be an excellent Random Thoughts blogpost. Wednesday (which is Thursday here in NZ but I’m still catering to my American homies!) will be the Topic of the Week, Thursday will be NSCA Tidbits, and Saturday will be an ABC (Ask Bret Contreras) post.
Some of you might remember an interview I did last September with Jurdan. He’s freaky smart and loves to talk shop. When I talk to him he’ll quote research like he’s Rain Man or something….”British Journal of Sports Medicine 2004 said…”, “McGill and colleagues blah blah blah.” The best thing about Jurdan is that he’s not afraid to speak his mind!
Jurdan is a co-owner of Zentrum Sports Rehab and Performace Center where many European athletes (especially soccer players) come to rehab. He is also a consultant in terms of rehab and injury prevention for European top profesional soccer teams. Jurdan is a European College of Sports and Exercise Physicians member (Hteam) and is dedicated to studying hamstring injuries.
Jurdan, how do you feel about the inner and outer core theory that many coaches and therapists (including myself) have regurgitated?
First off, let’s define the inner and outer core. I got this quote from one popular strength and conditioning coach that explains the anatomy and functions of the inner and outer core:
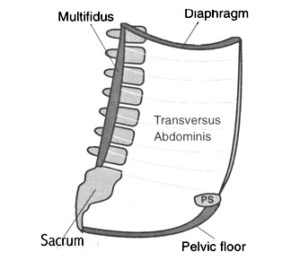
The inner core is like a cylinder made up of the pelvic floor as the base, the diaphragm as the top, the tranverse abdominis (TrA) muscle as the anterior border and the lumbar multifidus (LM) muscles as the posterior border. The function of the inner core is both physiological and mechanical as its main role is to provide the muscle activation required to sustain respiration, continence, and segmental spinal stabilization. Think of the inner core as your ‘reactive core’, meaning it should engage without thought in order to support outer core function. It acts as a stabilizer. Very critical point here, the inner core must engage, activate, or ‘fire’ prior to outer core or abnormal compensation patterns develop in movement resulting in possible injury.
The outer core is what most fitness professionals usually think of when talking about core training. The outer core is comprised of large multiarticular muscles such as the erector spinae, rectus abdominis, and the external oblique. The outer core provides postural stability, produces movement and resists external loads.
To summarize, inner core or local musculature = stabilizer and activates prior to movement and outer or global musculature = force producer and creates movement.
Research principally from Queensland University, elegantly directed by Dr. Hodges and expanded all over the world trough his famous book co-authored with Dr. Richardson entitled Therapeutic Exercise For Lumbopelvic Stabilization: A Motor Control Approach For The Treatment And Prevention Of Low Back Pain, claimed that local muscles or inner core (transverse abdominis, pelvis floor, diaphragm, and multifidi) fire in an anticipatory manner just milliseconds before the prime movers and exert the most important role to stabilize the spine at the segmental level. They infer that a dysfunction of those muscles and therefore motor control dysfunction are the principal factors for different pathologies and lack of core stability.
The finding that individuals with low back pain appear to have altered timing of feed-forward onsets of transversus abdominis reinforces the case for the presence of a motor control dysfunction. It is often inferred (NOT measured) that such a dysfunctional pattern corresponds to less than optimal core stability. Such an inference – that altered timing of the transversus abdominis leads to poor core stability – is popular between strength coach and clinicians but upon further inspection fundamental evidence is lacking.
In fact, recently an Australian Group has shown that the transverse abdominis does not always activates prior and symmetrically before extremity movement and states that feed-forward responses of the transversus abdominis are directionally specific and act asymmetrically (Allison GT et al 2008).
For example, Hodges et al. (1999) demonstrated that three of eight normal pain-free control subjects did not have feed-forward responses in 70% of trials during bilateral arm raising. Allisson G and Morris (2008) proposed that this is not due to ‘‘less than optimal stability’’ but rather a normal variation of motor control related to the lack of trunk rotation perturbation. Dr. Stuart McGill’s studies are also in line with these findings. In summary we cannot affirm that inner core musculature activates prior to the outer core or other muscles if we look to the evidence! To infer that a timing issue results in lack of core stability may not be accurate because is not directly measured. Now let’s look at what evidence says about its stability function.
Measuring stability is difficult and only a few labs around the world are able to measure directly and NOT inferred spine stability. I am unaware of a model that includes all of the core muscles (all muscles that inserts to the pelvis ) therefore we don’t really know core stability!
However, we can come close using a computerized model that consists of hundreds of modeled muscles fascicles, an electromagnetic tracking instrument used to asses kinematic data of each segment and synchronized to EMG. These are necessary to quantify each segment stability and all spine stability based in the potential energy approach (PE_1⁄2kx2). This approach allows us to calculate each segment stability and stability index of the entire spine. None of the studies using this approach show any particular influence of inner core muscles in stability. In fact Kavcic et al. (2004), when trying to assess the stabilizing role of individual torso muscles during rehabilitation exercises, concluded that no single muscle dominated in the enhancement of spine stability, and their individual roles were continuously changing across tasks. Clinically, if the goal is to train for stability, then enhancing motor patterns that incorporate many muscles rather than targeting just a few is justifiable.
From his numerous experiments, Dr. McGill claims that all muscles are necessary contributors to stability. Stability comes from a symmetric stiffness developed by the muscles around the spine. When a muscle contracts, it creates both force and stiffness. Stiffness results from muscle co-contraction and is always stabilizing. In contrast excessive force can compromise stability. Activating just one abdominal muscle would create just one source of stiffness but would also result in an interruption of the force linkage and when quantified, it would result in less stability (Grenier and McGill 2007).
There are not many randomized clinical trials that have been conducted but interestingly Koumantakis et al. (2005) compared the efficacy of many of the exercises that involve contraction of all the musculature with specific transverse abdominis and multifidus isolation. Adding the specific transverse abdominis training reduced efficacy compared to a more general program. The mode of action of stabilization retraining (transverse abdominis and multifidus) still remains unclear, because it has not been shown to be capable of mechanically containing an unstable segment, even upon improvement of muscle activation.
To summarize: it doesn’t appear that inner core muscles pre-activate in normal subjects or that the inner core muscles are the principal contributor to stability. All abdominal muscles participate in stability more or less depending the task. Yet myths and misconceptions regarding spine function persist and more research is needed in this area.
Wow, tell us how you really feel! Moving forward, what is your opinion about modern core performance programs in elite sports?
One of the problems today is that many clinicians and strength and conditioning coaches follow a “recipe” for assessment, treatment or performance training. Using this generic approach does not ensure optimal results.
In my opinion, when training for performance there is not much sense to inner or outer core work. I prefer to just look for demands of the sport, and through a biomechanical foundation and analysis adapt core work and its progressions to the individual profile AVOIDING any injury risk. In my opinion core work for a soccer player, track and field athlete, and basketball player shouldn’t be the same because the demands are different!
That makes sense. What do you think about actual rehab strategies for diagnosis and treatment in elite athletes?
Just for rehab there is a common mistake in practice focused in strength and flexibility training of the spine. Until today there in NOT a single study that shows a relationship between flexibility of the spine and low back pain and not clear association with strength exist. Moreover, a negative relationship has been shown (Parks et al. 2003, McGill et al. 2003). Take into account that a lot of stability is achieved in the first 25% of the maximum contraction level. Moreover, maximal muscle activity is observed during single-plane tasks, but muscle activation levels were constrained during functional tasks. Thus, strength training may not help muscles do what they need to do in “functional multiplanar” tasks. In my opinion we must assess patients’ intolerances to the different movements and forces and then build individualized programs that correct the disturbed motor patterns while avoiding undesirable loads. For this, you need to know each exercise’s biomechanical characteristics in terms of compression, shear, torsion, etc.
Jurdan, you feel that many coaches, especially coaches in the U.S., are hyper focused on one quality as it pertains to injury prevention. For example, many coaches think that the solution to hamstring tears is to simply get stronger hamstrings, or to simply increase hamstring flexibility. Please discuss why this view is limited and why we need to consider the entire picture and your idea of prevention.
This is not only a problem in the U.S.. Coaches here in Europe exhibit this same tendency – it’s all over the world. I will talk about my experience with European professional soccer teams. I cant see prevention as a couple of exercises to prevent each injury. I see prevention as a training system that needs programming, evaluation….etc. One part of the system could address general sport adaptations but the other needs to be individualized. Many years ago in Europe, conditioning coaches and physiologists in soccer were horrified when all the players did the same aerobic training at the same intensities. Nowadays each athlete runs at different intensities controlled by GPS or heart rate frequency. What happened in terms of injury prevention? Does each player really have the same needs and does every player really break down the same way?
Today all the players do the same work. Knowing that the success of a player is equal to his skill x availability (success= skill x player availability), and in lieu of recent reports show a loss of 40 million dollars in baseball teams due to injuries, I think that a change of direction related to injury prevention is needed, and this starts with coaches and team managers. In fact, I am accustomed to reading prevention training and injury matching as a first goal between the bigger strength coach but I’ve never seen a programmed system that as I see for strength or aerobic training . The interaction between aerobic, strength, neuromuscular control and mobility work must be taken into account in order to achieve success in injury prevention. Recently, for example, even though many people have discussed this issue in the past, for the first time a relationship between training loads and non-contact injuries has been developed. Therefore a program that control training loads looks impreative.
One of the problems of hyper focusing on only one quality could be derived from the actual research study designs that try to find direct cause and effect relationships without studying risk factors interactions. For example, the notion that lack of flexibility results in injury or lack of strength as injury predictor. The reality is that with this approach, hamstring strain epidemiology is the same as it was 22 years ago. We have the same amount of hamstring injuries or more. People tried to get recipes to resolve hamstring problems and we forget that for example 2, hamstring strains aren’t equal. It is too simple to do only one exercise to resolve a multifactorial injury as some research studies want to show. In strength training and conditioning we need to individualize the prevention process and integrate with the other areas to constitute an efective training system and know what each player needs. Using a generic approach ensures “average” results ,some players will improve and get better, but many will fail simply because the approach was not directed to address their deficits. For example, what happens in the hypothesis that biceps femoris is overstressed on account of a lack of lumbopelvic stability? Does the hamstring really needs strength or flexibility training? You may be need to address poor lumbopelvic stability first and foremost, and until this happens additional strength could be harmful for that athlete.
Do you feel that most coaches also have a “reductionist” view toward ACL injuries? What are some things that need to be taken into consideration when looking at ACL injury prevention?
Well, if we look at the scientific literature there is a relatively good amount of evidence showing that neuromuscular training can prevent ALC injuries in females (between 50-80 reduction in aveage). Normally this training consists of strength, balance, plyometrics, and core training but for example strength training alone doesn’t alter knee kinematics and moments post training (Herman DC 2008) and recently Powers et al. (2011) has shown that in contrast to strength, balance training increases cortical excitability. Therefore we need to know more about these training effects and strength is not everything as some strength and conditioning coaches may suppose.
About the reductionist approach, this is an approach used not only with the ACL, I think that it’s a general approach of research about musculoskeletal injuries as Carmen Quattman from Childrens Hospital elegantly addressed in a recent BJSM issue (Quattman C et al. 2009) where calls for a paradigm shift in methodology about prediction and prevention in musculoskeletal injuries.
Research has traditionally assumed a reductionistic view in order to explain injury aetiology or risk factors where a linear and unidirectional causal-effect model was systematically followed in many topics. This model is clearly influenced by the Western understanding of many phenomena and conceives any system as the sum of the parts. The medical understanding of the human body as an entity assembled from many pieces stems from Aristotle’s premises, showing the ancestral origin of this still current reductionist model. These parts are studied analytically in order to define the contribution of each one into the whole. Nowadays, there is no clear explanation or robust model that consistently demonstrates how all of the risk factors interact because a reductionistic model does not consider the interrelationships and random mixing of the parts.
For example, we assumed that the external knee abduction moment (>25Nm) was a predictor for ACL injuries in females in addition to reduced hamstring strength….. But lately some papers appear in order to explain injury mechanism from a more complex injury point of view. They talk about a complex interactions between risk factors in order for the injury to occur. They propose that decreased knee flexion angle together with a knee valgus torque could produce injury or not if concomitant knee laxity, dysfunctional muscle timing, and suboptimal tibial anatomy exist.
To put it another way, let’s say subject 1 and subject 2 have the same valgus torque and the same degree of knee flexion. Because subject 2 has a more shallow tibia, the probability of subject 2 suffering an ACL injury is much higher. As we see, valgus torque is not the only mechanism that can produce ACL injury. Recent research from Mclean et al. 2010 has shown a relationship between tibial anatomy and its influence on valgus. As you can see there are 2 different risk factors (anatomy and biomechanics) that influence each other.
* Editor’s Note: I sort of spoke about this in a Youtube video I created last year
In another example, knee laxity has been shown that affect timing of the hamstring muscles but the debate still remains in the literature as to whether the spinal reflexes are enough fast to protect ACL injury that occurs between the first 15 and 50 ms of the support phase.
In summary, interrelationships between many variables should be advocated which creates a more complex model in which all injuries are based in order to predict and prevent multifactorial injuries and obtain an accurate picture of the functioning of the body and ACL injury.
Thanks for the interview Jurdan!
My pleasure Bret. Take care.






Great interview. Jurdan knows his stuff. It is rare to find such objectivity.
Thanks
Craig
Thanks Craig! I agree. It is quite rare to find such objectivity.
Great article. I believe that the problem with a lot of generalized assessment programs is that they look at each muscle or even muscle group in isolation and not as a system working together. Strong core will do little if my entire pelvis(innominate) keeps rotating and (sacrum) torquing all at the same time! Perhaps my injury will be that much more serious as I will have a false sense of security and take on a larger laod.
Anyhow, I have a feeling that this topic is going to make me rant, so I am going to stop now! lol
Thanks for sharing,
Aggi
I agree Aggi. Of course many would consider all the pelvic muscles to be part of the core (some say pelvis to ribcage, some say knees to shoulders, etc.). And good call brining up the psychological aspect of injuries as it pertains to confidence! Thanks for the post!
Great interview, Bret! I enjoyed reading it and am glad to be reminded of the complexity of human movement. Reductionism may get the ball rolling, but it can give us a false sense of understanding by itself. That beIng said, measuring individual attributes of an athlete may tell us nothing, or worse, give us a false sense of optimism about our programs.
One thing I notice with clients is the quality or efficency of movement improves significantly. Their body learns how to navigate physical challenges better. You can see it in their gross movement patterns.
Exactly Dan. With good training everything improves….mobility, motor control, strength, power, etc.
Good stuff Bret!
I just heard about the earthquakes in NZ, hope you’re all good mate. Take care.
-Leigh from downunder!
Thanks Leigh. Everything is good here in Auckland. We didn’t feel a thing. Take care!
Hello bret, first time posting ( but I’m your reader from the beginning of your wordpress blog ).
Even if your articles are kinda long, I don’t find them boring as other articles ( as I read quite allot ) I must say you have your thing when it comes to keeping the audience on the article.
Also I have a question for you :
1. It seems that after yesterday’s training ( squat 5×5, bench,row) <- when I was out from the gym I felt ok, but when I got home and got down in a squat position to check something, I felt like I pulled my right hamstring.
It doesn't hurt when I don't contract it, and when I do contract just a little sore and maybe a little "pulled" muscle, what should I do ( Tomorrow I want to do deadlifts ) can I do them or should I skip them ?
Florin, this is a blogpost of its own…..but there’s no way to know until you wake up in the morning. Sometimes things feel completely better, sometimes they get worse, etc. So just go by how you feel, and listen to your body. Of course the safest method is to take a couple of days off regardless, but not many strong lifters have that mentality. Interesting that your hammie acted up while in a squat position….they don’t get stretched much in a squat due to the biarticular nature. If it keeps occuring, you need to figure out why it’s happening (hip flexibility…weakness….etc.). Best of luck!
Finally a guy with a mind of his own. Who else is tired of the wannabe PTs that can’t get anyone in shape? Movement quality doesn’t mean wimpy exercises. Movement quality is my morning dump. Freak Factory!
Jesus Bob! Tell us how you really feel. 🙂
The best coaches can get people freaky strong with good form and understand how to clean up movement patterns while still training hard. I admit that I’m tired of some of the PT’s who have never gotten anyone strong, but I have learned a ton from them. Hopefully they’ll start learning a ton from us too.
Awesome post, thanks both of you. We have a long way to go to abandon the reductionist approach in training and rehab, but it’s encouraging every time I read an article like this. I look forward to more, and to the nest step of programming with this philosophy.
Great interview!
Very enjoyable read Bret. Always like someone that can speak their mind, and also have the Rain Man memory quality to back it up. Rare to find indeed!
Thank you peeps!!! Glad you liked the interview.
Hi Bret,
totally off-topic. I heard about the earthquake in NZ and I just wanted to make sure that you are okay. You are in Auckland, right?
Bianca
Bianca, yeah, I’m in Auckland. All is good here! No worries. Thanks for the thoughts.