






Recent Posts / View All Posts
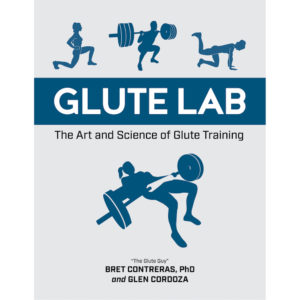
Here are the podcasts that I've been a guest on in 2023: Movement Optimism with Greg Lehman - Dr. Bret Contreras takes on movement technique, social media and critical thinking…
Here are the podcasts that I've been a guest on in 2023: The Obvious Choice with Jonathan Goodman - Surviving and Growing in the Fitness Industry with Bret Contreras Phil…
Here are the podcasts that I've been a guest on in 2022: Escape Fitness - Bret Contreras | Muscle Building, Glute Training & the Latest Research The Shane Walsh Podcast -…
Here are the podcasts that I've been a guest on in 2021: Avrora's Podcast - V.B.TALKS with "Glute Guy" - Bret Contreras EPISODE #23 (video HERE) Dr. Swole's Podcast - Bret Contreras: Glute…
Here are the podcasts that I've been a guest on in 2020: The More Than Fitness Podcast - Bret "The Glute Guy" Contreras, PhD — What's Missing From The Current State…
Here are the podcasts that I've been a guest on in 2019: Mind Pump Podcast - Bret Contreras- The Glute Guru The Mind Muscle Project - Bret Contreras on The Science of…